All across the world, the population of older people is increasing, but there are so many barriers that make it challenging for them to age gracefully and with dignity. Technological advancements and medical strides have increased longevity, putting much-needed pressure to reform our healthcare system. According to the World Health Organization, 1 in 6 people will be aged 60, an estimated 1.4 billion people globally, and our current healthcare system is unprepared to care for the complexities that aging brings to our heterogeneous society. (World Health Organization, 2023). The issues have been amplified since the COVID-19 pandemic as more people have developed chronic issue or their current health issues have been exacerbated. Barriers to integrated care for older adults should concern us since they significantly impact our economy and quality of life.
Barriers such as gaps in the quality of adequate integrated care stem from social determinants such as transportation, education, and income. (Jones & Dolsten, 2024). This is especially evident in the rural part of the country, where older adults are often isolated and have limited access to providers for all their physical and mental health needs. According to the World Health Organization, older adults are at a high risk of developing mental health conditions such as depression and anxiety due to many factors, such as isolation from reduced mobility, chronic pain, chronic health problems, and inadequate care as well as lack of natural or professional support. These stressors increase the rate of isolation and loneliness, with an estimated 27.2% of deaths from suicide. (World Health Organization, 2023).
Older adults who require long-term care, such as those with a progressive dementia diagnosis, are often discouraged during the eligibility process, especially when they do not have the necessary resources to navigate the tedious process to meet the requirement for Long Term Care Medicaid. The process can take weeks, months, or even a couple of years to decide. In such instances, the caregivers or families of older adults, if any, also face tremendous frustrations navigating the system. The lengthy process can increase unnecessary institutionalization and rampant emergency room visits, negatively impacting our economy and society due to misuse of resources.
With the increase in privatization of health insurance, many who joined the managed care or Medicare advantage bandwagon have to jump through hoops when they need services such as acute in-patient treatment or procedures. Providers often complain about adequate reimbursement, especially in rural areas, leading to fewer providers willing to provide services in these areas. The litigation of reimbursement also leads to some services, such as in-patient psychiatric care, ending abruptly to avoid the risk of insurance denial. Lack of adequate health literacy is another barrier to quality and holistic, integrated care for older adults. Most places in rural areas must travel quite a distance to visit their primary providers or practitioners for disease management. In instances where there are multiple morbidities of illness, the lack of frequent wellness checks can lead to poor health literacy, which increases the rate of emergency room visits, inadequate care, and, sometimes, traumatic experiences for the patient.
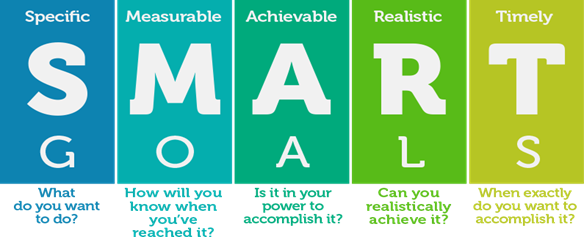
With the barriers mentioned earlier to integrated healthcare for older adults and more that I cannot cover in this column, I would like to address this issue in a few ways. Our goal as a society as we move forward should be person-centered care to improve our quality of life and healthy aging. (Fulmer, Reuben, Auerbach, Galambos, & Johnson, 2021). We can start by laying the foundation for universal healthcare to replace our current healthcare system. As practiced by our counterparts in developed countries, universal healthcare systems have successfully provided equitable care. It would save the country money and boost our economy. We should strengthen public health’s role by developing and implementing new approaches to health care delivery through evidenced-based policy changes such as the NY SO 5516 bill. (The New York State Senate, 2023). We should review our existing policies and assess how feasible they are to our current societal needs regarding adequate healthcare, especially for our aging population. We should allocate resources to achieve patient-centered care focused on the needs of our aging population, such as more infrastructure for palliative and end-of-life care that does not always need to be in nursing homes.
The World Health Organization (WHO) and the U.S. Centers for Disease Control view aging through a holistic lens, including social connections and living environments that contribute to the health and well-being of older adults. Even though increased longevity is considered a benefit, it is clear that the solutions associated with aging-related issues are limited. (Lane, Palley, & Shdaimah, 2020, p. 189). Our current healthcare system is an excellent example of a lack of infrastructure, and it will not be able to support the projected increase in the older adult population by 2030. Establishing an adequate and effective healthcare system will ensure older adults age gracefully and with dignity to improve their quality of life
References
Fulmer, T., Reuben, D. B., Auerbach, J., Galambos, C., & Johnson, K. S. (2021, January 21). Actualizing Better Health And Health Care For Older Adults. Health Affairs, 40(2), 219–225. doi:10.1377/hlthaff.2020.01470
Jones, C. H., & Dolsten, M. (2024, May 10). Healthcare on the brink: navigating the challenges of an aging society in the United States. NPJ Aging, 10(22), 1–9. doi:10.1038/s41514–024–00148–2
Lane, S. R., Palley, E. S., & Shdaimah, C. S. (2020). Social Welfare Policy In A Changing World (1st ed.). Sage Publication Inc.
The New York State Senate. (2023). Senate Bill S5516A: 2023–2024 Legislative Session. Senate Bill, Mental Hygiene Law, New York City. Retrieved from https://www.nysenate.gov/legislation/bills/2023/S5516/amendment/A
TIMMINS, A. (2024, August 29). Patients ready for discharge languish in New Hampshire hospitals, taking up needed beds. New Hampshire Bulletin. Retrieved from https://newhampshirebulletin.com/2024/08/29/patients-ready-for-discharge-languish-in-new-hampshire-hospitals-taking-up-needed-beds/
World Health Organization. (2023, October 20). Mental Health of Older Adults. Retrieved from World Health Organization: https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults